What Is SIBO?
What is SIBO?
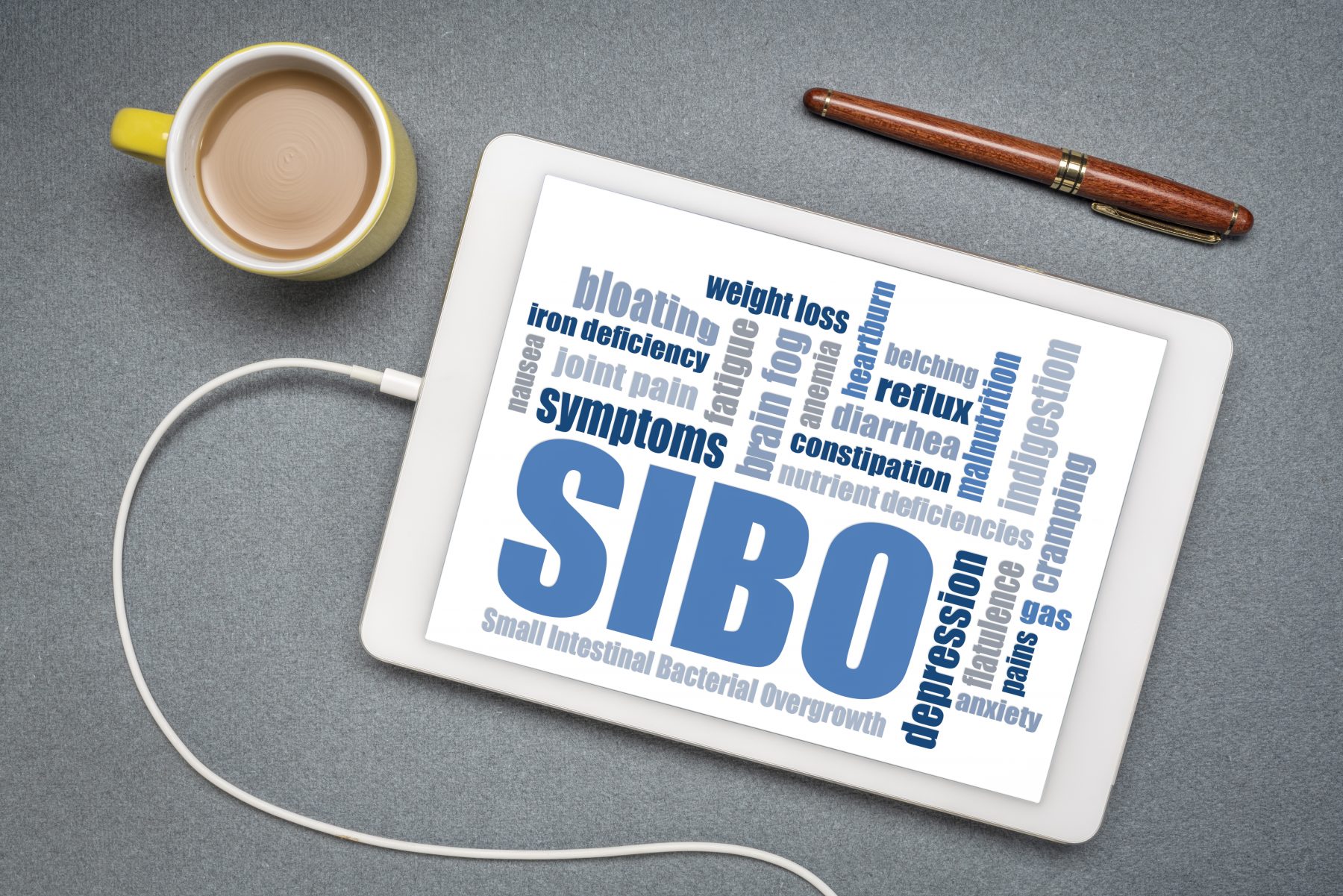
SIBO, small intestinal bacterial overgrowth, is defined as an increase in the number of bacteria, and/or changes in the types of bacteria present in the small bowel. In most patients, SIBO is not caused by a single type of bacteria, but is an overgrowth of the various types of bacteria that should normally be found in the colon (1). Less commonly, SIBO results from an increase in the otherwise normal bacteria of the small bowel.
SIBO has been shown to negatively affect both the structure and function of the small bowel. It may significantly interfere with digestion of food and absorption of nutrients, primarily by damaging the cells lining the small bowel (the mucosa). Additionally, this damage to the small bowel mucosa can lead to leaky gut (when the intestinal barrier becomes permeable, allowing large protein molecules to escape into the bloodstream), which is known to have a number of potential complications including immune reactions that cause food allergies or sensitivities, generalized inflammation, and autoimmune diseases (2).
Risk factors for SIBO
- Low stomach acid
- Irritable bowel syndrome
- Celiac disease (long-standing)
- Crohn’s disease
- Prior bowel surgery
- Diabetes mellitus (type I and type II)
- Multiple courses of antibiotics
- Organ system dysfunction, such as liver cirrhosis, chronic pancreatitis, or renal failure
SIBO can be responsible for autoimmune conditions that patients are given limited options for treating. SIBO can cause pain and discomfort. However, this condition is very treatable. Lowering inflammation in the gut is one of the most preventative ways we can assure long term health. A SIBO work up is warranted anytime we are experiencing a condition in which inflammation plays a roe, from IBS to weight gain, SIBO should be ruled out. Treating SIBO can result in symptoms resolving and remission occurring, however you can’t treat what you don’t know you have.
